Ophthalmology Billing and Coding Tips
Billing and coding are essential to running a thriving ophthalmology practice. While there are certain billing and coding situations that are unique issues for ophthalmology as a specialty, practices must also keep general regulatory requirements in mind. In this blog, we’ve compiled some ophthalmology coding tips from various industry organizations.
Choose carefully between Eye and E/M codes when billing for eye examinations
Where can I find Eye codes?
Eye codes refer to CPT codes that document new and established eye exams, most commonly found between 92002 and 92014.1 Eye codes are used for both routine and medical visits in ophthalmology.
Where can I find E/M codes?
E/M codes stand for Evaluation and Management codes.2 These are used to bill professional services such as physician and nonphysician practitioner clinic visits, hospital visits or consultations, and are most commonly found between 99202 and 99499. E/M codes are used across all medical specialties.
Determine your ophthalmic procedure code type
When determining whether to use an Eye code or an E/M code, it’s important to consider the level of service performed, which will help determine whether the exam was intermediate or comprehensive. Note that as of January 1, 2021, level of service is determined by either medical decision-making or physician time. For more information on determining which codes to use, visit the American Academy of Ophthalmology website.3
Be sensitive to the risks of out-of-network billing
The No Surprises Act increases patient protections against surprise billing
On September 30, 2021, the Centers for Medicare and Medicaid Services issued an interim final rule called “Requirements Related to Surprise Billing; Part II.”4 This rule provides increased protections from surprise medical bills for patients with job-based and individual health plans. These protections apply when receiving emergency care from out-of-network providers, as well as in certain nonemergency situations. With increased regulatory scrutiny on out-of-network billing practices, it’s more important than ever to be vigilant when a patient’s medical insurance lists your practice, or a certain provider, as out-of-network.
The new rules also will require healthcare providers to provide uninsured or self-pay patients with good-faith estimates of expected charges for scheduled services. If billed charges are substantially in excess of the good-faith estimates, providers may have to participate in an independent patient-provider dispute resolution process.
Nontransparent billing practices could harm patient satisfaction
According to IBM, more than half of US patients don’t understand the healthcare system well enough to navigate benefits and services effectively.5 Patients may get frustrated and choose to go elsewhere for their care if they receive a bill that they do not expect and cannot understand or pay.
Transparency in your billing services is key to preventing patient frustration. Patients may not understand what their medical and vision insurance will cover. Ophthalmology practices can provide helpful explanations via handout or on their websites to help patients understand the difference, building trust through transparency.
Understand differences between payers
Billing guidelines differ between federal and commercial plans
Getting familiar with the most frequent payers for your patient population will help you keep track of coding guidelines, which can be important to make sure you don’t miss out on reimbursement options. Certain commercial payers will limit billing frequency for Eye visit codes, as well as place restrictions on what types of eye diagnosis codes you can use.6 However, E/M codes are usually not subject to such frequency restrictions.
Create a payer spreadsheet
Creating a payer spreadsheet helps you track and compare reimbursement rates for your top commercial payers, along with Medicare, for your most commonly used examination codes. Here is an example from the American Academy of Ophthalmology.7
Ensure you always have human eyes on code selection
Train providers on proper documentation and coding procedures
It’s important for physicians to receive proper coding training on a regular basis, as well as notification and training on the annual code updates. Risk cannot be determined by an EHR-suggested coding function, because providing care to a patient involves clinical and human nuances that computer functions cannot yet capture. Therefore, the provider and billing and coding staff must always review the selected or suggested code for accuracy. EHR-suggested coding functions are meant to facilitate correct selection, not take the place of it.
Do not undercode to avoid an audit
Undercoding is the practice of selecting codes that fail to capture the scope of work performed.8 Frequently a simple oversight, some practices undercode on purpose because they believe it will reduce the chances of an audit. In reality, undercoding results in a skewed data pattern, which can raise alarms for payers. Also, your practice risks potential lost revenue from underreporting your scope of work.
Almost everyone may be audited at some point. The best way to proceed is to keep current on coding best practices and support everything you do with proper medical documentation.
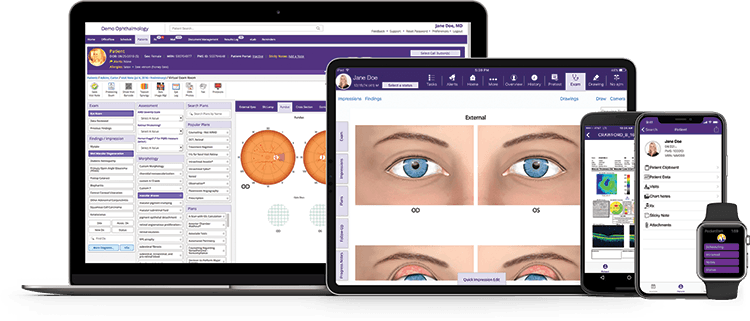
How ModMed® Ophthalmology can help
When using ModMed Ophthalmology, code suggestions are based upon clinical documentation in conjunction with protocols. Protocols wrap commonly seen diagnoses, treatments and more into a single touch to help providers document quickly. When a protocol is applied, the EHR automatically generates a suggested code based upon the documentation. When clicked, a rationale explaining factors for the code’s selection appears. Details affecting code selection and modifiers are always manually editable.
It’s important to remember that the ultimate legal responsibility for coding lies with the practice. You always need to ensure that the code you select reflects that the services provided are medically reasonable and necessary before you finalize the visit. However, EHR software that’s built for ophthalmology can help you ensure you have supporting documentation.
Our ophthalmology team members can help you explore automatic suggested coding and other helpful billing features to determine if ModMed Ophthalmology is the right solution for your practice.
1 AAPC: The “Eyes” Have it: Routine vs. Medical Eye Exams, November 2, 2012.
2 AAPC: What Are E/M Codes?, November 4, 2020.
3 AAO: Eye Visit vs. E/M Codes: What a Difference a Code Makes, July 16, 2019.
4 CMS: Overview of rules & fact sheets, November 26, 2021.
5 IBM: What is healthcare price transparency?, 2021.
6 AAO: How to Choose Between E&M or Eye Codes, March 3, 2017.
7 AAO: E&M or Eye Code: Which to Choose?, January 1, 2015.
8 DukeHealth: Steps to Avoid Overcoding and Undercoding, July 30, 2019.
The materials included in this blog were current as of December 9, 2021 and may be subject to change. Updates and details on the topics contained herein may be available from the CMS, the CDC, and other commercial payers. Modernizing Medicine makes no warranty regarding the ongoing accuracy of the information provided.
This blog is intended for informational purposes only and does not constitute legal or medical advice. Please consult with your legal counsel and other qualified advisors to ensure compliance with applicable laws, regulations, and standards.




