Urology Coding Do’s and Don’ts: Guidelines For Best Practices
Billing and coding is one of the most important aspects of running a urology practice. But it can be a confusing process, especially for people who aren’t professional coders. We’ve taken the guesswork out of basic urology coding with these guidelines, so that anyone can understand how it works.
Section 1 – Urology Coding Basics
Select the right code in less time
There are three main categories1 to consider when performing CPTⓇ coding for urology: Evaluation and Management (E/M) Codes, Procedure Codes, and Add-on Codes.
- E/M Codes: E/M stands for Evaluation and Management codes. These are used to bill professional services such as physician and nonphysician practitioner clinic visits, hospital visits or consultations, most commonly found between 99202 and 99499.
- Procedure Codes: These codes refer to those used to bill for diagnostic and treatment services, most commonly found between 50010 and 58999.
- Add-on Codes: These codes identify procedures carried out in addition to the primary procedure. In the CPT manual, these are designated with the “+” symbol. These codes may be payable if reported with the appropriate primary procedure.2
Knowing these general categories and where you can easily find them can narrow down the field considerably when selecting a code. Once you know what type of code you’re looking for, the chart notes should identify the diagnoses and procedure(s) performed to help you pick the best option by providing essential details of the services completed for the patient on that date of service (for example, Diseases of the Genitourinary System are ICD-10 codes from N00-N99).
Sweat the small stuff
For example, in cases involving a bladder cancer diagnosis, you should always check the procedure notes for the location from which the bladder tumor was removed. One common mistake is overusing C67.9,3 bladder cancer unspecified. An unspecified diagnosis should only be used when the information in the medical record is insufficient to assign a more specific code. It would be extremely rare that there would be no mention of the location of the tumor removal in the procedure notes, so your claim could come back rejected due to unspecified coding.
Examples of codes with more specificity:
C67.2 Malignant neoplasm of lateral wall of bladder
C67.3 Malignant neoplasm of anterior wall of bladder
C67.4 Malignant neoplasm of posterior wall of bladder
C67.5 Malignant neoplasm of bladder neck
This frustration and duplication of work can be avoided. Remember, coding must be supported with proper documentation, but code selection must take the documentation into account during first selection. Otherwise, you could run the risk of missing small but important details that could result in claim rejection.
Section 2 – Urology Coding Do’s and Don’ts for a Smooth Billing Experience
Do always have human eyes on code selection.
Risk cannot be determined by an EHR-suggested coding function.4 Therefore, the provider and billing and coding staff must always review the selected or suggested code for accuracy. EHR-suggested coding functions are meant to facilitate correct selection, not take the place of it.
Do train providers on proper documentation and coding procedures.
It’s important for physicians to receive proper documentation and coding training on a regular basis. Providing care to a patient contains nuances that billing and coding staff are not trained to capture because they’re not clinically trained. Providers must be involved in selection and review.
Do not undercode to avoid an audit.
Undercoding is the practice of selecting codes that fail to capture all work performed.5 This most often happens simply due to oversight, but some practices purposely do it because they think it will reduce the chance of an audit. Undercoding results in lost revenue due to work not being reported, but it also results in a skewed data pattern. That’s a big red flag for Medicare, because they’re actively looking for deviations to investigate.
Almost everyone will be audited at some point in their careers. The best way to proceed is to keep staff current with training on coding best practices and support everything you do with documentation.
Section 3 – How ModMed® Urology Handles Coding
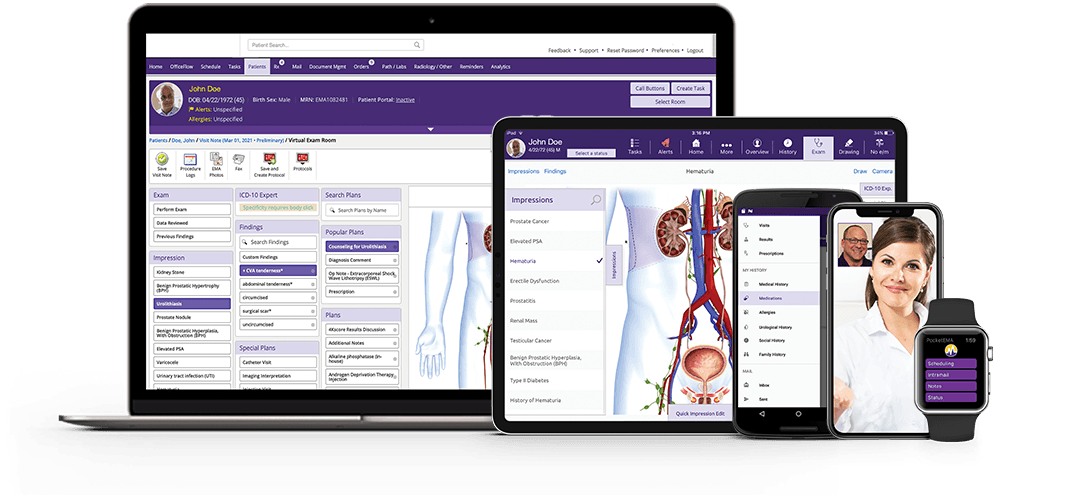
When using EMA®, you can dictate as much of the note as you see fit and manually input the Medical Decision Making (MDM) level if you prefer. Or, you can use a quick tap-through Exam function that utilizes structured data to pick up on MDM factors and suggests codes to you. The code suggestion is based upon your documentation in conjunction with Protocols. Most modifiers are included within the coding functionality of EMA.
Protocols wrap commonly seen diagnoses, treatments, orders and more into a single touch to help the provider speed up documentation. When a protocol is applied in the note, EMA automatically generates a suggested code based upon the documentation. When clicked, a rationale explaining factors for the code’s selection pops up. For example, using a protocol for a visit to evaluate a prostate nodule may suggest an E/M code of 99212, then allow you to modify details including nodule features and location.
It’s important to remember that the ultimate legal responsibility for coding lies with the practice, not the software. You need to have human eyes on the code selection and supporting documentation to ensure you’re covered when an audit occurs.
Details affecting this code selection are always manually editable. For example, the status button shown to the right of the exam will show the Presenting Problem Complexity sub-window, from which you can edit the Medical Decision Making factor without leaving the Virtual Exam Room (VER).
Let’s say the Risks of Complications were slightly more complex than usual. Documenting additional information in this area of the MDM may increase the level and could change the E/M code, depending on other factors you’ve documented during the visit.6 The encounter form and note includes the pertinent supporting documentation you need to justify the code to payers stored within EMA.
Remember that EMA’s suggested codes are just that – suggestions. You always need to ensure that the code you select reflects the medical documentation and that the services provided were medically reasonable and necessary before you finalize the visit.
Commonly seen cases in urology coding
Let’s say you’re seeing a patient for a possible vasectomy. Best medical practice is generally to perform one consultation and then the procedure at a later date, giving the patient time at home to consider all risks and benefits of the procedure. That could be one E/M code (for the consultation) and one Procedure code (for the vasectomy), billed separately on different dates of service.
But what happens when you need to bill more than one category of code in a single visit? For example, a patient presents with an abscess that requires immediate removal. An evaluation is performed and the provider decides the procedure must happen immediately to protect the health of the patient. How do you code these events appropriately?
EMA can recognize these situations based upon the documentation and also with the Separate & Identifiable Plan under the Plan tab. This option can be used when an E/M code and Procedure code must be billed out of clinical necessity. It captures the information needed to justify multiple categories of services occurring in a single visit.
Useful coding functions in EMA for urologists
The Override Billing function can be accessed after a note is complete and before it is finalized. This function brings up the full MDM calculation for you to review and modify if needed. Additionally, you can bill by time from this option if you choose. Simply input the total time spent with the patient on that calendar day and select the associated activities you performed from a pregenerated list or by using free text, then select Bill By Time.
The ICD-10 Expert function helps decrease claim denials due to lack of specificity, and it will automatically pop up when certain diagnoses are selected that often require a further layer of specificity modifier. For example, selecting “hematuria” in EMA will prompt the ICD-10 Expert to open, asking the user what kind of hematuria the patient is experiencing and capturing code specificity. Claim denials slow down your accounts receivable and are a pain to reconcile. This function can result in an increase in cleaner claims moving forward.
EMA’s coding functions can help providers and staff to save time during the day, and can help lower your practice’s audit risk by supplying appropriate fields, factors and information for editable supporting documentation.
It’s important to remember that the ultimate legal responsibility for coding lies with the practice, not the software. You need to have human eyes on the code selection and supporting documentation to ensure you’re covered when an audit occurs.
You can explore automatic suggested coding and other helpful coding functions for your practice with one of our urology team members.
1 Urology Times: Beware of these 3 common ICD-10 mistakes, October 16, 2018.
2 CMS.gov: Add-On Code Edits, September 16, 2021.
3 ICD10Data.com: 2022 ICD-10-CM Diagnosis Code C67.9, 2022.
4 Urology Times: Urology practice do’s and don’ts for proper billing, April 29, 2019.
5 Duke Health Referring Physicians: Steps to Avoid Overcoding and Undercoding, July 30, 2019.




