Benefits of Telemedicine in Pain Management
“Everything that can be digitized will be digitized. And it will happen before you know it.” — Kara Swisher, The New York Times1
Once upon a time, we commuted to offices to work, attended schools to study, shopped in stores to buy stuff, and visited doctors’ offices for treatments. Then came a devastating worldwide pandemic and an explosion of technological innovation. Telehealth pain management systems, integrated with pain EHR systems, were among those breakthroughs, which became keys to what was dubbed “the new normal.”
Prepandemic, the healthcare establishment resisted telemedicine for pain management, so the field was ripe for disruption. But today, those who run our complex and expensive healthcare systems are embracing cost-effective new ways of increasing productivity for practices and providing continuity of care for patients.
Early Days of Pain Management Telemedicine
![]() Telemedicine and telehealth debuted well before the 2020 lockdown challenged the continuity of care for pain patients and the ability to operate for pain practices. For example, in the late 1960s, Massachusetts General Hospital introduced the first hospital-based, multispecialty telemedicine practice, offering remote clinical exams at Boston’s Logan International Airport.2
Telemedicine and telehealth debuted well before the 2020 lockdown challenged the continuity of care for pain patients and the ability to operate for pain practices. For example, in the late 1960s, Massachusetts General Hospital introduced the first hospital-based, multispecialty telemedicine practice, offering remote clinical exams at Boston’s Logan International Airport.2
Before the COVID-19 public health emergency, however, telehealth pain management was a bit more complicated. Medicare generally limited reimbursement to rural areas. Patients still had to travel to medical facilities, called originating sites, and physicians were not permitted to practice from their homes. State and federal laws and regulations restricted treatment across state lines, the prescribing of medications based on telehealth, and the types of licenses needed to practice electronically.
Evolution of Telemedicine for Pain Management
Telehealth and telemedicine had been developing and showing evidence of efficacy. Then in response to the 2020 public health emergency (PHE), they suddenly became essential. The International Association for the Study of Pain and the American and European Associations of Regional Anesthesia and Pain Medicine urged the integration of telemedicine pain management into routine clinical care.2
Government agencies waived certain rules during the PHE, allowing the use of private audio and video technologies, potentially transforming the field.3 Medicare lifted certain restrictions during the PHE, allowing providers to be reimbursed for telehealth visits (synchronous audiovisual communications) as they would for office visits.4 By December 2020, Medicare had added another 144 telehealth services to be covered through the end of the emergency.5
 Some states waived or reduced licensure requirements that had prevented providers from treating patients in other states via telemedicine, and they loosened other requirements to make it easier to prescribe medications remotely. The Drug Enforcement Administration allowed practitioners to prescribe controlled substances for legitimate medical purposes without first conducting medical exams in person, as long as audiovisual communications were interactive in real time and practitioners complied with applicable state laws.4
Some states waived or reduced licensure requirements that had prevented providers from treating patients in other states via telemedicine, and they loosened other requirements to make it easier to prescribe medications remotely. The Drug Enforcement Administration allowed practitioners to prescribe controlled substances for legitimate medical purposes without first conducting medical exams in person, as long as audiovisual communications were interactive in real time and practitioners complied with applicable state laws.4
The Office of Civil Rights, responsible for protecting the privacy of patient information, loosened its enforcement of penalties for providers who acted in good faith but used certain non-HIPAA-compliant technologies during the emergency.4
For 2022, Medicare’s Physician Fee Schedule promotes greater use of telehealth to expand access to behavioral health care, especially in underserved communities. Conforming to recent legislative changes, the rules eliminate geographic barriers and allow patients to access telehealth services from their homes for the diagnosis, evaluation and treatment of mental health. Counseling and therapy services, including substance use disorders and opioid treatment programs, should be more readily available.6
How Telehealth Pain Management Helps Your Practice
With modern telemedicine for pain management, providers can interview and observe patients, take histories, collect treatment records, deliver education, monitor requests for opioids, and issue prescriptions, subject to applicable laws. They can also conduct behavioral interventions like stress management, modifying thoughts, and physical activity.
According to a 2020 review in the journal Pain, follow-up visits can be conducted both virtually and effectively.3 In another Pain review, cognitive-behavioral therapy techniques via telehealth emerged as potentially helpful not only for managing pain but also for mitigating the emotional distress of the pandemic.7
A 2021 review in Pain Reports concludes that pain management telemedicine has improved patient compliance, satisfaction and quality of life. Patients accessing telehealth-supported services feel more confident and empowered, and they experience better relationships with medical staff.2
By the end of 2021, a report from the US Department of Health and Human Services, which analyzed Medicare fee-for-service data, found massive increases in the use of telehealth during the pandemic, with behavioral health providers seeing the highest utilization. Medicare visits via telehealth increased 63-fold, from 840,000 in 2019 to 52.7 million in 2020.8
 Going forward, we can expect the benefits of telehealth for pain management to continue. Medicare announced it would eliminate geographic barriers permanently and allow patients to access telehealth services from home for the diagnosis, evaluation and treatment of mental health disorders. Other services allowed temporarily during the emergency would remain in place through December 31, 2023, while Medicare evaluates whether to add them permanently.8
Going forward, we can expect the benefits of telehealth for pain management to continue. Medicare announced it would eliminate geographic barriers permanently and allow patients to access telehealth services from home for the diagnosis, evaluation and treatment of mental health disorders. Other services allowed temporarily during the emergency would remain in place through December 31, 2023, while Medicare evaluates whether to add them permanently.8
However, the requirement that patients present to an originating site to receive telehealth services will resume once the PHE expires if Congress fails to pass permanent telehealth legislation, advocated by a bipartisan group of elected officials.9
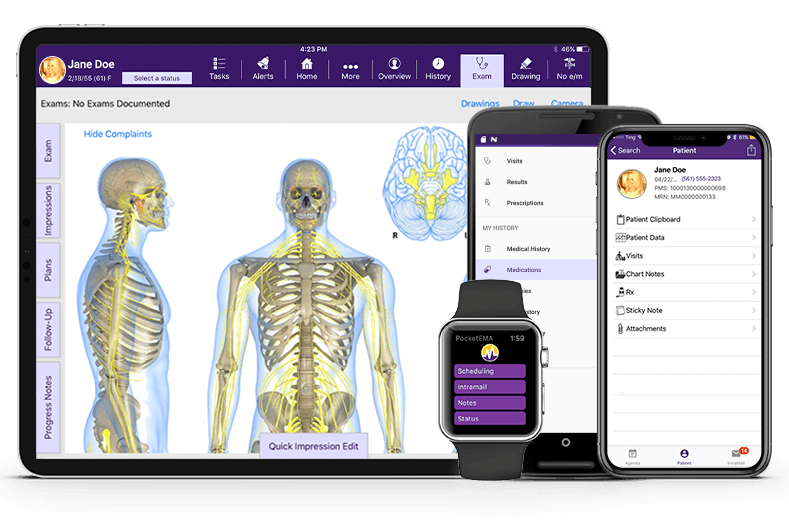
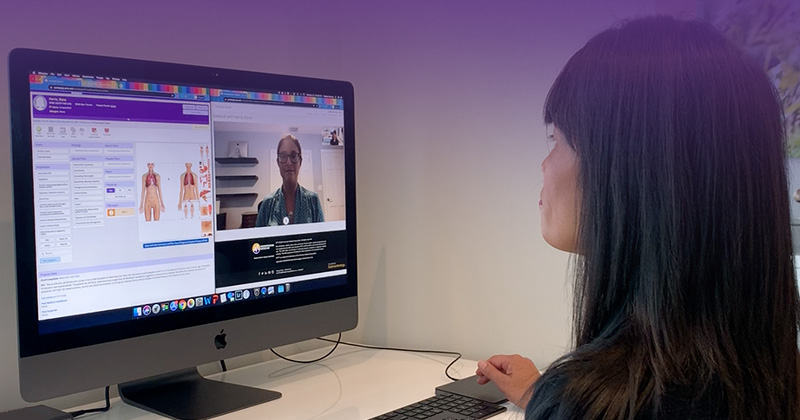
Early in the pandemic, ModMed® Pain Management incorporated new synchronous telehealth capabilities into its cloud-based pain EHR software, EMA®. Rapid deployment via the cloud helped pain patients to continue treatments and pain practices to continue operations, all while reducing the risk of transmitting SARS-CoV-2.
Reference
1. Kara Swisher, “Another Big Step Toward Digitizing Our Lives,” The New York Times (2021 March 19), www.nytimes.com/2021/03/19/opinion/NFTs-beeple-crypto.html?action=click&module=RelatedLinks&pgtype=Article
2. Jordi Perez, et al., “Telehealth and chronic pain management from rapid adaptation to long-term implementation in pain medicine: A narrative review,” Pain Reports (2021) 6(1): e912, www.ncbi.nlm.nih.gov/pmc/articles/PMC8108593
3. David J. Tauben, et al., “Optimizing telehealth pain care after COVID-19,” Pain (2020 Nov) 161(11): 2437–45, www.ncbi.nlm.nih.gov/pmc/articles/PMC7566302
4. “Key Telemedicine Reimbursement and Guideline Changes,” Blog, ModMed (2020 April 16) www.modmed.com/blog/telehealth-key-guideline-changes
5. “Trump Administration Finalizes Permanent Expansion of Medicare Telehealth Services and Improved Payment for Time Doctors Spend with Patients,” PR, US Centers for Medicare & Medicaid Services, US Department of Health & Human Services (2020 December 1) www.cms.gov/newsroom/press-releases/trump-administration-finalizes-permanent-expansion-medicare-telehealth-services-and-improved-payment
6. “CMS Physician Payment Rule Promotes Greater Access to Telehealth Services, Diabetes Prevention Programs,” PR, US Centers for Medicare & Medicaid Services, US Department of Health & Human Services (2021 November 2) www.cms.gov/newsroom/press-releases/cms-physician-payment-rule-promotes-greater-access-telehealth-services-diabetes-prevention-programs
7. Christopher Eccleston, et al., “Managing patients with chronic pain during the COVID-19 outbreak: considerations for the rapid introduction of remotely supported (eHealth) pain management services,” Pain (2020 May) 161(5): 889–93, www.ncbi.nlm.nih.gov/pmc/articles/PMC7172975/
8. “New HHS Study Shows 63-Fold Increase in Medicare Telehealth Utilization During the Pandemic,” PR, US Centers for Medicare & Medicaid Services, US Department of Health & Human Services (2021 December 3) www.cms.gov/newsroom/press-releases/new-hhs-study-shows-63-fold-increase-medicare-telehealth-utilization-during-pandemic
9. Kat Jercich, “Dozens of U.S. legislators push for telehealth coverage expansion,” Healthcare IT News (2022 January 31), www.healthcareitnews.com/news/dozens-us-legislators-push-telehealth-coverage-expansion
This blog is intended for informational purposes only and does not constitute legal or medical advice. Please consult with your legal counsel and other qualified advisors to ensure compliance with applicable laws, regulations and standards.




