Four Secrets to Help Towards ENT MIPS Success in 2019 & Beyond
Learn how otolaryngology MIPS works, why it exists, and how you may be able to help set up your practice to succeed
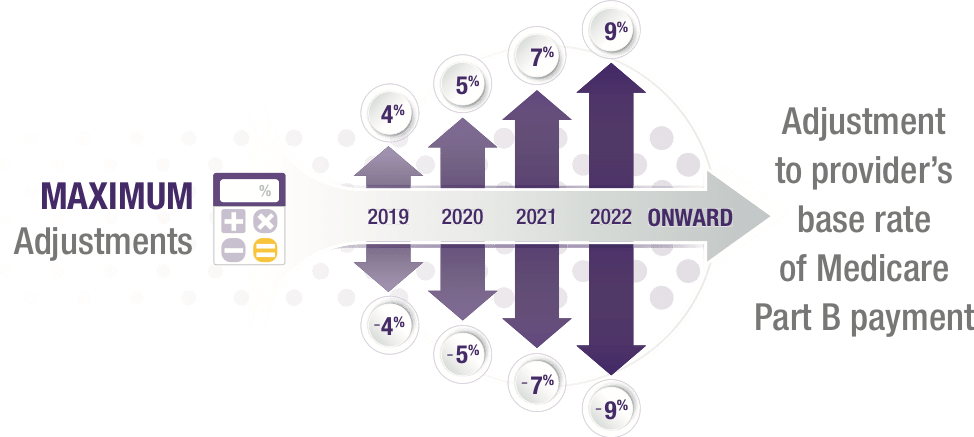
With thousands of pages of Quality Payment Program (QPP) regulations released every year, the Merit-Based Incentive Payment System (MIPS) for ENT can be more than a little confusing. The stakes keep getting higher, as the maximum negative adjustment to your Medicare reimbursement is currently expected to increase to 9% in 2022 (based on 2020 performance), up from 7% in 2021 (based on 2019 performance).
If you’re looking to participate for the first time, or to make successful participation a bit less overwhelming, keep reading. We’ll give you a crash course in the history, purpose and structure of MIPS for otolaryngology, as well as teach you our top recommended strategies that can help you succeed.
By understanding how to streamline ENT MIPS participation, you may be able to help relieve a good deal of the reporting burden—while helping your practice stay on track to potentially earn up to 7% more on covered Medicare services.
Table of Contents:
- Background: What Are MIPS and MACRA?
- How Does ENT MIPS Reporting Work?
- Four Secrets to MIPS Success for Otolaryngologists
- Final Thoughts
Background: What Is MIPS, and Why Was MACRA Created?
At its most basic level, the MIPS program, which is one component of the Centers for Medicare and Medicaid Services’s (“CMS”) Quality Payment Program (QPP), combines elements of three separate incentive programs – Meaningful Use (MU), Physician Quality Reporting Program (PQRS) and Value-Based Payment Modifier – that have been increasingly used by the Centers for Medicare and Medicaid Services (CMS) in the last several years in an attempt to drive change in the way health care is provided to patients. The fundamental goal of all these programs is the same: incentivize providers for delivering high-quality care and reducing costs, rather than just the amount of services they provide. This concept is known as value-based care.
MU was established in 2009 by the Health Information Technology for Economic and Clinical Health (HITECH) Act, passed by the Obama administration as part of the American Recovery and Reinvestment Act of 2009 (ARRA) economic stimulus bill, to support the adoption of electronic medical record technology across the healthcare continuum. CMS also created similar incentive programs known as the Physician Quality Reporting System (PQRS) and the Value-Based Payment Modifier (VBPM), in an effort to increase the focus on the quality of patient care.
With each program, providers had to collect data on designated measures, then submit that data to CMS. CMS generally paid incentives, and in some instances imposed penalties, based on a provider’s participation in the program (e.g., meeting minimum reporting requirements) and performance against established metrics. In many instances, the programs relied purely on incentives in early years of development, transitioning to more substantial penalties the longer a program was in existence. For example, providers who performed well enough might be eligible to receive a positive adjustment to their Medicare fee-for-service payments, while those who failed to achieve adequate levels of participation or performance could receive a negative adjustment, decreasing their income for the year.
These programs all aimed to help improve outcomes and cost-effectiveness, with each targeting a slightly different aspect of those goals. However, it was quite complicated for physicians to have so many separate programs, so CMS ultimately lumped them together into MIPS as one of two tracks in its new Quality Payment Program (QPP).
The creation of the QPP had been mandated by the bipartisan Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), and it replaced the Medicare Sustainable Growth Rate (SGR).
When MIPS took effect in 2017, it made value-based care a reality on a scale never seen before in the US. The program is still in early phases and CMS is working up to full MIPS implementation in 2022, so the full impact to the health care system, both for patients and for providers, has not yet been experienced.
Although the scope of the program continues to evolve, and we’re still in the early years of the incentives and penalties it establishes, MIPS can already have a big impact on your bottom line. MIPS payment adjustments are made by CMS based on a provider’s MIPS score in the performance year two years prior to the current payment year. So, for example, your practice’s Medicare reimbursement for 2019 was adjusted by up to 4% based on your performance in the 2017 performance year. For performance year 2019—which will impact your 2021 reimbursement—the payment adjustment increases to 7% and, if no other modifications are made to the program, the payment adjustment for the 2020 performance year and beyond, which will modify reimbursement starting in 2022, will increase to 9%. That means that if you bill $1,000,000 in Medicare next year, your MIPS performance could make a $180,000 difference in your 2022 income depending on how you perform.
So for many otolaryngologists, the question is not whether to participate, but how to participate most effectively. In fact, otolaryngologists are even more likely than the average physician to participate in MIPS—46% planned to participate in 2019 compared to 37% across all specialties.
How Does ENT MIPS Reporting Work?
Now that we understand the history behind this incentive program and why it’s so important to participate, let’s look at some of what MIPS requires. A complete explanation of the program, including all performance measures, can be found here.
First of all, it’s important to determine whether or not you are eligible to participate in MIPS. This depends on factors including how many Medicare patients you see and how much you bill in Medicare charges. Some exempt clinicians also have the ability to opt in and qualify for the payment adjustment, an ability which CMS added for the 2019 performance year. To help you determine whether you are eligible for MIPS for 2019, you can use this lookup tool from CMS.
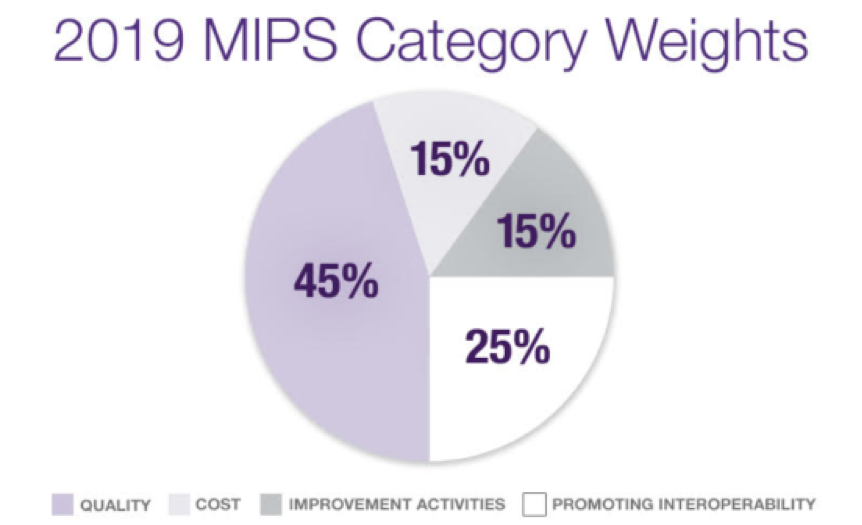
Similar to the three prior value-based care incentive programs it combined, MIPS requires providers to collect and submit data on designated measures. In fact, MIPS incorporated each of the existing programs into its own MIPS category (with significant modifications).
MU became Advancing Care Information, now known as Promoting Interoperability, which focuses on patient engagement and the electronic exchange of health information using certified electronic health record technology (CEHRT). PQRS became Quality, which aims to promote quality of care based on performance measures created by CMS and by medical professional and stakeholder groups.
The Value-Based Modifier, meanwhile, became Cost, designed to gauge the total cost of care during the year or during a hospital stay. CMS also introduced a fourth category, Improvement Activities, which focuses on improving care processes, enhancing patient engagement and increasing access to care.
Each category has different requirements for how many measures must be reported and how many points each measure is worth. They change every year, and can be found on CMS’ Quality Payment Program website.
Each category also has an overall weight, with the allocation changing from year to year, and together, they add up to create a final otolaryngology MIPS Composite Score. The highest possible score is 100, but not every provider needs to aim quite that high.
To avoid the negative adjustment, you simply have to meet the minimum MIPS performance threshold, which is 30 points for 2019. If you earn more than 30 points, you may receive a positive payment adjustment.
There’s also an exceptional performance threshold, which is currently 75 points. If you score above 75 points for 2019, you’ll be eligible for a share of an exceptional performance bonus pool in addition to your positive adjustment. The program’s requirements and minimum performance thresholds are being phased in over time and, so far, most participants have qualified for the positive adjustment.
However, the ultimate goal of MIPS is to compare physicians to their peers, so beginning in performance year 2022, the rules as currently drafted contemplate that performance thresholds will be set at the mean or median of prior performance. As such, this would mean that if you score above average, you would 2018 QPP Participation Results Infographic (4), but if you score below average, you would receive a negative adjustment. This could make it harder to succeed than under the current calculations.
Providers are not currently required to report to CMS on all measures and, in some categories, are able to select the metrics that are most relevant to their specialty and practice. A complete list of the metrics for each category can be found on CMS’s QPP website. Once you’ve decided which measures to report, you can determine which reporting methods to use. CMS now allows clinicians to submit through a wide variety of different methods, including MIPS CQMs, EHR reporting and direct attestation. In addition, you can report as an individual, a group or a virtual group depending on whether you meet certain specifications. For up-to-date details on reporting, visit the CMS website.
If you’d like to know more about the 2019 requirements, explore our breakdown of what’s changed in MIPS for 2019.
Four Strategies to Help You Achieve MIPS Success
We’ve looked at why ENT MIPS was created and how it works, but how can you make it simpler for your practice to work towards achieving success? Here are our top tips.
1. Use an EHR that can automate much of the work
When collecting your ENT MIPS data, you don’t want to disrupt your workflow by having to enter the data in multiple places and go out of your way during the exam workflow. That’s the trouble with many EHRs out there—they don’t recognize your quality measure data.
However, some EHRs are based on structured data and can automatically recognize data entered within the flow of the exam as usable for MIPS. This can help save you a lot of time and clicks. To speed things up even more, these systems may be able to help to compile your MIPS data for submission automatically and even allow you to submit it through their own ENT MIPS Qualified Clinical Data Registry (QCDR).
This can help save you the trouble of having to submit it manually, and can make it easier to submit all your reportable categories in one place.
2. Track and benchmark your estimated score on a daily basis
ENT MIPS is all about how you’re performing compared to your peers, so it’s important to have an easily accessible dashboard that makes it easy to track your progress. You have enough going on without having to worry about tracking MIPS manually in a spreadsheet or having to log into another system and re-enter data to see your score. It’s simplest to use a tool that’s built right into your EHR system.
You also want to make sure you’re choosing the right measures from the outset. A good MIPS dashboard can break down all the measures for you and help you figure out which ones may make the most sense for your practice. Then, you can select your desired measures, see what you need to do to achieve them and track your estimated progress on a daily basis. You can even drill down to the patient level to see which patients are failing or passing each measure.
If you’ve started to fall behind, you’ll be able to see your data, so you can make appropriate workflow adjustments to catch up again.
3. Get support from Certified ENT MIPS Advisors
Even with the best technology, it can be tricky to keep up with everything, and there’s sometimes no replacement for having a knowledgeable person to talk to.
That’s why some vendors offer otolaryngology MIPS advising services. They can pair your practice with a Certified MIPS Healthcare Professional (CMHP) who can help to train you on MIPS, help you set goals for your practice and create a plan of action to help you get there. Along the way, they can monitor your progress, meet with you periodically and answer your questions to help keep you on track.
If the MIPS advising service is provided by your EHR vendor, your MIPS advisors can even provide guidance on how to use the EHR system to help you collect the right data. And then when it’s time to submit, they can guide you through step by step to help streamline the process.
4. Find a trusted vendor who has your back
When looking for the tools and support that can help you succeed in MIPS, it’s important to partner with a company that has a great deal of experience in otolaryngology value-based care. Specifically, look for a record of successful past submissions and experience in reporting otolaryngology quality measures.
The truth is, it’s not just about the technology; it’s about the people behind it. If you can get all of your ENT MIPS products and services together as part of an all-in-one solution that combines people, processes and technology, you’ll have that many fewer logins, clicks and phone calls to deal with. If you know that those solutions are powered by a trusted, established vendor with whom you have a good business relationship, you can feel more confident and more prepared to navigate MIPS both now and in the future.
Final Thoughts
Understanding and navigating otolaryngology MIPS can be complicated, but it can be important for your bottom line—and it will only become more important in coming years. The good news is, if you have access to the right tools and support, you can make it much easier to work toward achieving ENT MIPS success. Because the truth is, it’s not just about the score or the incentives—it’s about being free to focus on your patients and grow your business.




