Eye Codes versus E/M Codes: A Guide to Ophthalmology Billing
E/M code updates may see some ophthalmologists revisiting when to use them
For many ophthalmologists, the use of eye codes instead of evaluation and management (E/M) codes has been the default for many years. Practices can choose which code structure they use on a case-by-case basis, but many professionals have historically preferred the simplicity of eye codes.
Now, in the wake of an E/M codes overhaul, there may be scenarios where ophthalmologists and their billing teams prefer to use E/M codes over eye codes. Here, we’ll review some of the details related to the shift, so you can discover what may work best for you.
The Background on Switching Codes
It’s a unique situation that ophthalmologists have two ways to bill.
In the 1980s, the Academy of Ophthalmology worked with the Centers for Medicare & Medicaid Services (CMS) to develop a separate code structure — the eye codes most ophthalmologists use today.
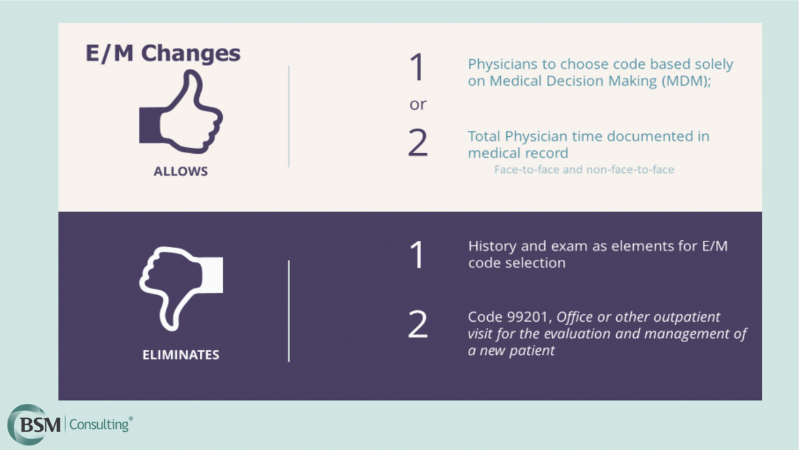
Ophthalmologists rarely used E/M codes before January 2021 because the documentation was burdensome. However, when the documentation requirements changed, ophthalmologists started using E/M codes for billing more frequently.
Eye Versus E/M Billing Criteria
While ophthalmologists and their billing teams should review criteria independently, here is an overview of documentation requirements:
- If you decide to use eye codes, the criteria have not changed. You’ll include documentation of history, general medical observation, and chief complaint, as well as any required examination elements and diagnostic and treatment programs.
- If you decide to use E/M codes, you’ll need to include documentation of the patient’s medically appropriate history and/or examination, plus your code selection, based on either medical decision-making or total physician time.
It’s worth noting that, alongside the evolution of billing processes, some ophthalmology CPT codes are changing for calendar year 2023 and may require teams to review and update their documentation. For instance, there are many new time codes that may apply to your work.
Billing Prompts: Ophthalmology practices that use ModMed® benefit from the provision of code prompts that may help with billing. These prompts show estimated billing amounts for comparison. Ophthalmologists and their billing teams may wish to be strategic in discovering the most appropriate approach for their practices.
When to Use E/M Codes for Eye Visits
It can be helpful to have a working understanding of which codes to use when. Here are a few scenarios where you might use E/M codes over eye codes:
- When the number of patient visits exceeds the payer’s allowance for eye codes
- When payers require E/M codes for medical diagnoses
- When payers downcode based on diagnosis
- When payers allow for E/M consultation codes
- When visits qualify as telemedicine visits
- When place of service is an emergency department
- When total physician time is prolonged
Outside of these scenarios, you may find that you still use both code structures across your practice. The revamp of E/M code documentation requirements just means they may be a more frequent choice.
Ophthalmology Billing in ModMed
ModMed EHR workflows can help support your final determination of which billing code to use.
During patient visits, you and your team provide inputs related to patient complaints, observations and other details. You can also see a side-by-side comparison of reimbursement values for E/M versus eye codes with tabular information on each calculation.
By working in ModMed during patient visits, your practice can explore the optimal code for the care you provide on a case-by-case basis. For more on ophthalmology billing or to see ModMed in action, book a demo.
This blog is intended for informational purposes only and does not constitute legal or medical advice. Please consult with your legal counsel and other qualified advisors to ensure compliance with applicable laws, regulations, and standards.







