Helping to Maximize Patient Engagement Tools

How to elevate patient engagement at your medical practice
In a recent webinar, Relatient CEO Michele Perry and Modernizing Medicine®’s Director of EMA® Ophthalmology, Dr. Michael Rivers, discussed mobile-first strategies towards winning at digital patient engagement.
Have you ever found yourself wondering:
- What drives gaps in patient engagement?
- What is a digital front door and how can it help my practice meet our business objectives?
- What are some success stories of practices that are solving for patients and have experienced success?
- How can I get through the day more easily and increase staff efficiency?
- I want our practice to become more patient centric, but how do I get started?
If you’ve had these questions cross your mind, then tune in to the recorded webinar or read the post below. Michele and Dr. Rivers share their experiences and the importance of creating a digital front door strategy for your practice.
What is a digital front door strategy? Where do patient engagement tools fit into the mix?
Historically, healthcare has been location-based, but patients, especially in the digital age we live in, are no longer location-based. There’s a disconnect. The concept of a digital front door strategy bridges the gap with increased mobile access and proactive outreach to take a patient-centric approach.
Physicians spend a majority of time obsessing over clinical workflows and ways to optimize them. Similarly, they focus on improving the business side of the practice as well. The third component, which has taken a back burner, is the patient communication aspect. This piece has been more challenging until recently.
So what’s driving the shift to collaborate more with patients than in the past? If we think of patients as consumers, which they should be, expectations from healthcare align to our expectations from other consumer-driven companies. Take Amazon or Uber for instance. Both provide the end users instant communication. Ordering new household supplies or ordering a ride to your destination are naturally woven into our lives, as both are accessible on the go via smartphones.
We all expect virtually instantaneous communication, so why shouldn’t the same ring true in healthcare? The good news is that we’re starting to see a shift in the right direction, in part because patients are demanding it from their healthcare providers and tools have been developed to answer this demand.
Providing patients with access to self-service capabilities and mobility can help build loyalty, especially among digital natives. Patients’ expectations for digital tools from healthcare providers are only going to continue to grow.
As with any change to the status quo, the shift to patient-centered engagement has been difficult. Why? In the past, there has been a lack of tools. Practice staff would spend hours on the phone for follow-ups or send snail mail to remind patients of appointments and get them back in the door. Neither approach has ever been efficient for the practice or the patient, but now we have technology tools to help automate and streamline these processes.
Like any business, medical practices need and want to maintain relevancy and competitiveness. Without a strategy to work toward or improve the digital front door, practices risk falling behind in both.
What are some benefits of digital patient engagement?
Some benefits of improving patient access and driving a patient-centered, mobile-first strategy can include:
- Reducing no-shows
- Driving patient compliance
- Collecting patient payments faster
- Enhancing office efficiency
- Increasing patient retention and loyalty
- Improving patient satisfaction
- Expanding patient access
- Attracting new patients
 Let’s look at reducing patient no-shows with help from tools such as automated patient reminders. It’s a medical issue when patients don’t come back, but also an issue in your revenue stream. Remedying this issue benefits both patients and the practice. Patients should receive the care they need, and the practice can keep a full schedule. By solving issues the patient encounters, it will pay off for your practice, too.
Let’s look at reducing patient no-shows with help from tools such as automated patient reminders. It’s a medical issue when patients don’t come back, but also an issue in your revenue stream. Remedying this issue benefits both patients and the practice. Patients should receive the care they need, and the practice can keep a full schedule. By solving issues the patient encounters, it will pay off for your practice, too.
For instance, an appointment reminder can be sent via text, email and voicemail, helping to maximize the communication platforms where the patient could be reached. It fits into their day-to-day routine. The ability to confirm, cancel or reschedule directly from the reminder without having to create a username or password makes adoption of the platform that much more seamless. You want to communicate to patients where they are, and for many, that’s via their smartphones.
It’s about providing the care patients need without costing the practice.
Results: The Tools to Measure Patient Engagement
As a practice, how do you know if the steps you take to increase digital patient engagement are working? Measure results. Here are two case studies showing how that can be done.
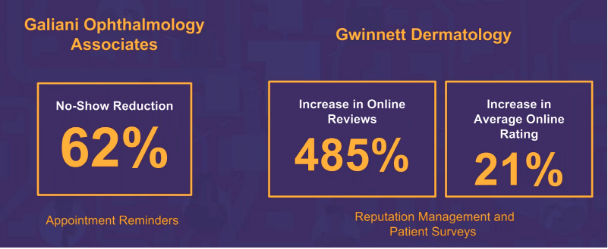
Galiani Ophthalmology Associates needed assistance in reducing no-show rates. They had their staff making manual patient phone calls to remind patients of appointments. It just wasn’t working. It drained employees and cost them significant revenue. They needed a solution that was easy for both patients and clinic staff to utilize. After implementing appointment reminders, the practice saw a 62 percent relative reduction in no-shows and now has a 1.7 percent no-show rate, both exceptional results.
Also, let’s look at Gwinnett Dermatology. The practice knew it needed to increase its online presence and understood the importance of online reviews. It needed a good way to solicit patient feedback in as close to real-time as possible and make the practice discoverable online. After implementing reputation management and patient surveys, the practice experienced a 485 percent increase in online reviews and a 21 percent increase in average online ratings. As patients are increasingly turning to the internet to make decisions on providers, this will only grow in value and importance for practices to remain competitive and relevant*.
What are some driving factors behind patient engagement tools?
We have seen four big shifts affecting healthcare organizations that should help drive the approach for a digital front door.
- Patient experience and satisfaction
- Patient access
- Financial responsibility
- Adoption
Patient Experience and Satisfaction
There’s often a disconnect between what physicians think their patients experience and what patients really think. Why? It used to be all one-way communication. The physician would tell the patient all the information with little questions or input from the patient. It was a one-sided conversation.
This has since shifted, which is a very good change for both parties. Now, more than ever, patients are more involved in their healthcare decisions. And taking a patient-centric approach can help physicians hone their skills, too.
Patient Access
Patient accessibility still poses a challenge in all healthcare settings. So what contributes to long wait times and overwhelmed patients? We can place partial blame on the convoluted marketplace. Patients have their primary care physicians, specialty providers, a clinic at CVS or even urgent care clinics. They oftentimes are unsure of where they are supposed to go for what, especially if they can’t easily get in touch with a provider to ask questions.
The other factor is a lack of communication tool technology. Waiting on hold for great lengths of time when trying to schedule an appointment or confirm results just isn’t efficient for either party. If we give our clients better tools to communicate with practices and vice versa, it gives patients more clarity. Without automated tools, it’s been a challenge for practices to effectively manage waitlists and often, they have come up short on filling last-minute openings.
Financial Responsibility
Patients continue to experience increasing financial responsibilities, and fewer patients pay their full portion of the bill. Practices need to be better equipped to collect copays and balances at the time of service or work with their patients on a payment plan. Outstanding balances may lead to a patient skipping follow-up appointments.
Communication tools need to come into effect to understand what the barrier was for the patient’s lack of return and if it was a financial one. Communication about financial responsibility should include dialogue between patient and practice. If a central billing office calls the patient to collect, there is no connection or personalization. They’re disconnected from where the actual care took place. It’s integral to integrate clinical, business and patient engagement cycles to have coordinated messages.
Patients often give up and then don’t show when they can’t get in touch with the practice or face a financial hurdle. It’s important for the patient to be heard by the practice. It comes down to providing more than just clinical care—it’s about providing customer-service.
Adoption
When the status quo is challenged, there’s always a level of pushback. A way to have both practices and patients adopt new technology is to fit it into their current workflows and daily schedules and add convenience.
The overarching goal is a simple one. Let’s end the dreaded (and inefficient) game of phone tag.
Maximizing Your Staff Time
Without automated tools, staff must call patients during the workday for appointment reminders meaning they can’t focus their time on the current in-office patients. When patients come in for care, it extends beyond just seeing the doctor. Patients often need to schedule a follow-up, go through billing conversations and understand their treatment plan. A good medical practice will make sure the patient has multiple touchpoints with office staff to make sure all the information is conveyed. If staff is on the phone making calls, this creates a barrier and detracts from the in-office patient experience.
Practices that use the right combination of automation and personal, human touch, excel at engaging practices. Take a standard automated text reminder for instance. The initial message and response to the patient may be automated, but the staff can actually respond back if needed via text or can help triage if a call is needed. There should still be a person on the other end. Technology should help to augment efficiency, but it is not a replacement for personal touch.
Starting the process of adding patient engagement tools to your practice.
So how do you start the process of evaluating and rolling out digital patient engagement technology? This can certainly seem overwhelming.
Here are some tips to start.
- Determine the right people who should be involved in the evaluation and vetting process.
- Decide on a champion at the practice to help successful adoption.
- Figure out how patients interact with your healthcare organization currently.
- Ask: What do we currently do? Do we have current automation? How mobile-friendly are we?
- What patient touchpoints are the most important and why?
- How do we measure success once automated tools are implemented?
When you are evaluating vendors, here are some helpful hints:
- Find and work with an expert in the space. Select a vendor that has the clinical, business and patient engagement aspects covered.
- Look for a vendor that has a track record of happy companies and industry expertise and results to help guide you.
- Make a matrix and evaluation tool to evaluate demos and capabilities of vendors and various patient engagement tools.
Conclusion
At the end of the day, you want to provide your patients—aka the consumers—with a positive experience, and that expands beyond the clinical side of your practice. Using the right patient engagement tools and technology can help you take customer service to a new level in the digital age in which we live. Patient engagement tools provide the foundation for a strong digital front door strategy, benefiting your practice, your staff and your patients in more ways than one.
*Individual results may vary




