The State of Gastroenterology Technology Post-Pandemic
Running a gastroenterology practice, and running it well, is no small feat. The COVID-19 pandemic emergency and subsequent shut down brought operational difficulties, burnout and staffing shortages. While the specialty is beginning to recover, longer term value-based care trends, such as changing reimbursement rates and medical coding updates, are still in play.
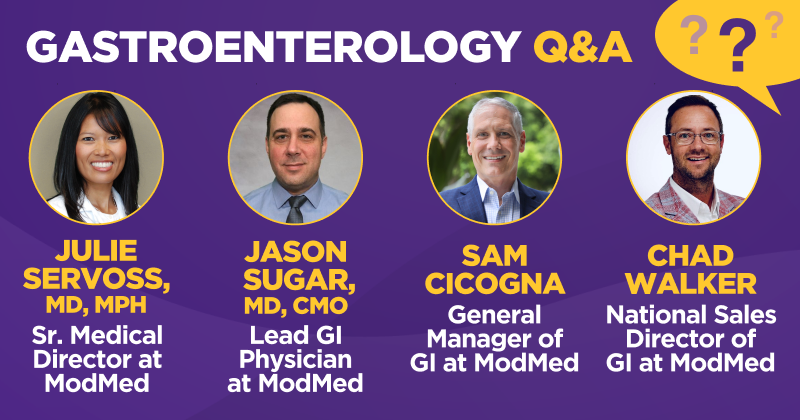
We asked a panel of ModMed® Gastroenterology physicians and gastroenterology healthcare technology specialists how technology has evolved to help practices adapt to both rapid shifts and longer-term changes.
The interview below has been edited for length and clarity.
ModMed: In your experience, what has been the most significant technological challenge for gastroenterology practices?
Sam: First of all, many practice staff are not tech people, they’re healthcare professionals. They don’t necessarily have full-time tech people on staff. Also, after new tech has been purchased, the implementation and training part is often an afterthought. Assuming people will eventually figure it out costs time and ROI. Some of this is complicated, and you need that specialist to teach you how it works, otherwise it slows you down. It can be a huge limiting factor to making the most of your investment.
Chad: I would add that there’s a significant amount of investment that people don’t usually think about on a daily basis. In some cases, software features are being paid for, but not being utilized to their full potential. If they were, you might not feel as burned out, because you’d be able to leverage these tools to help yourself. That’s a big miss.
ModMed: How has the technology used in gastroenterology practices changed over the past five years?
Sam: I think that Patient Engagement technology has taken a major step forward. Everything’s mobile now, and the patients are expecting an easier, more seamless experience, so the tech has naturally followed behind it.
Chad: Five years ago we were introducing software to ASCs. Clinics were already incentivized to adopt software through meaningful use, but ASCs were still trying to figure out ways to automate pre- and post-op care. Everybody felt like their software didn’t talk to each other; now we’re seeing more communication between systems.
Dr. Servoss: I think from a private practice standpoint, physicians were forced to rapidly adopt virtual check-in and telemedicine when the pandemic hit. Physicians aren’t always known for being good with change, but the pandemic showed us that we can change rapidly if we need to.
The notion of innovation in gastroenterology is well accepted, and I think large practices are beginning to see that they may have to leverage technology even more. There’s a huge demand for patient self-scheduling to manage scale. As physicians, we’ve had to acknowledge we need to let go a little bit and free up human beings to do the really critical communication.
Dr. Sugar: Telemedicine had been limited to somewhat rural areas prior to the public health emergency, and now it’s expanded. Smartphone apps have proliferated in the past five years for chronic disease management and overall health. Now patients have access to a wide variety of apps that they can use to help manage chronic diseases, along with wearable technology for remote patient monitoring.
Additionally, AI has expanded a lot in the past five years. Applications in the GI space include computer assisted polyp detection and identification of research candidates. There is also interest in staging disease severity for Barrett’s esophagus and inflammatory bowel disease.
Can you describe the emotional impact of using outdated technology on gastroenterology physicians?
Chad: If you have to come in early and stay late, it takes a toll on your personal life. If you’re always bringing work home, you might be missing out on your kid’s swim meet. But the note has to get done, or you don’t get paid. In the office, if you’re behind on the schedule, and then you add new tech on top of that with inadequate training, you’ll likely get notoriously behind. Change is hard, it can create fear for practices. They’re either afraid to look and see what’s out there, or they’re afraid they’re going to be forced into changing.
Sam: On top of that, they’re being rated online on a public forum by their patients. You can see that one person that says, “I saw Dr. Sam and he didn’t have time for me.” That’s a lot of pressure to perform, and I think emotionally it can get transferred into frustration with the technology. When your normal workload is so stressful on a daily basis, you’re not necessarily thinking about how to make things better.
Dr. Servoss: It feels overwhelming. That’s the life of a physician. The more you do, the more you get paid. It’s a safe profession in that you’re always in demand, but we’re trained that if there’s more to do, you just do it. That doesn’t change the fact that there are only 24 hours in a day, and this is one reason why burnout happens. We love seeing patients and making medical decisions, but that’s encased in all of this administrative work. A high percentage of your time is spent on managing the administration of the patient, not talking to them. So how do we leverage tech to decrease that burden for physicians and staff? If we can save as much of that time as possible, the staff is freed up to support the physicians, and that’s a win. That’s where tools such as gMobile™ and patient self-scheduling can really help.
Dr. Sugar: I’ve personally seen how using outdated tech contributes to decreased job satisfaction and morale. It also increases the risk of burnout for medical staff, because there are so many inefficient, manual processes. Anything that helps automate data entry can help ease administrative burden in the practice.
ModMed: Can you describe the business effects of using outdated technology?
Sam: It all comes down to time. If you’re not seeing as many patients, you’re not getting paid for as many patients. Then there’s the revenue cycle management part of it, and understanding what makes your revenue cycle efficient. If you don’t understand your RCM, you’re quite possibly missing claims entirely. And if you don’t understand the MIPS reporting requirements, you could be missing out on MIPS reimbursement as well, which is going to have a business impact.
Chad: Reimbursement rates are tricky. So you may have to figure out how to keep your practice profitable year to year beyond seeing patients, whether that’s by finding new revenue streams or making sure you’re getting correctly reimbursed per encounter based on your notes. But if you’re still using outdated tech, your infrastructure may prevent you from doing either. If I have to make phone calls to patients to try to fill my schedule, that may be inefficient. If you know how to use tech to solve those issues, you’re on the road to improving practice success and improving patient outcomes.
Dr. Sugar: I talk to people and sometimes they’re still on paper charts. Sometimes their EHR isn’t fully integrated, so they have staff working in multiple systems at once. Before we went live with gGastro® in 2014, we had a separate EHR, an endowriter, a scheduling module and a billing module. So you had front office staff working in three or four systems at a time, and the physicians would have to work in two systems at a time. That’s very inefficient. Having a fully integrated EHR and practice management system can eliminate a lot of inefficiencies.
ModMed: In your opinion, how can these technologies improve processes to help with staff retention?
Chad: I believe the most important change is eliminating disparate systems. A single solution is paramount. You need to get to a point where you only have to key in the data once, and it’s shared from your clinic to your ASC, and to the billing department. Beyond having a single solution, there’s so much you can do, instead of just blindly letting your calendar fill up and hoping for the best. Now we have marketing solutions to set up a website and manage web presence. There are also analytics tools that can help you monitor how often your sickest patients are coming in so you can see if they’re getting regular care.
Sam: I think our population is at a place where people are aging out of the workforce, and it’s creating a situation where you can no longer hire 20 people to man the phones, because you can’t find them. Instead, you can use technology and have one person handle multiple patients. Maybe use patient engagement technology to set up texting for patient reminders. Letting the patients schedule their own appointments on the web, and then having a staff member validate them can save so much time over manual scheduling. Making sure your open appointments are out there on the internet for patients to find on their own, all of that technology is available right now to help.
Dr. Servoss: I think COVID really strained staffing. It was difficult to find good managers, medical assistants and PA’s before the pandemic, and I think COVID lit a fire under that. It was hard to keep people, and those who are left are burned out. We have to be more strategic in thinking about how we keep our people happy and developing. Sometimes it just gets boring doing the same thing 50 times per day. Perhaps a change in the rhythm can break up the monotony. If you’re cross trained in scheduling, authorizations, patient support, and education, you can rotate people and get them refreshed. But you need to save time to cross-train them.
If you have things like patient self-scheduling, maybe you don’t need two full-time schedulers, maybe you only need one. If self-scheduling is working great, and I see that prior authorizations for medications is taking too long per patient, I can train that staff member to support prior authorizations and smooth out that process. It’s about using people in a more efficient way
.Dr. Sugar: I think the answer is different depending on your practice’s situation. Ask yourself what tasks are ripe for automation. Is your office staff still calling patients to remind them of their appointments? You could use gReminders™ to send out an automated message instead. Are you using a staff member to send out patient satisfaction surveys when it could be going out automatically? You could use gSurveys™. Is your staff scheduling everyone over the phone? Consider putting a system in place to allow patients to self schedule online.
ModMed: What are some up-and-coming technological advancements that we can look forward to in the gastro space?
Sam: AI applications are still really early in terms of development. There are some applications out there that are starting to make headway. Right now it’s focused on the procedures. I think we’ll see AI come through that’s finding patients that are good matches for your practice, and that can look at and analyze patterns in population health. It’s starting down that road, but we’re not there yet.
Chad: My head goes to an individual health record that’s translatable anywhere. There’s tech out there where I can use robots to pick up on my speech patterns and transcribe it, but the next big leap would be hearing what I say and then planning for it. For example, if I’m a physician and I tell the patient verbally that I want to see them back in two weeks, the system would start the scheduling process. But it’s not quite there yet. It doesn’t have the context. When AI starts to understand the important data points, then we’ll really make leaps and bounds.
Dr. Servoss: GI is really at a great place for adopting new tech and thinking about machine learning and how that can help us, especially when it comes to screening for colonoscopies. We haven’t automated colonoscopy prep education for patients. Screening colonoscopies are so standardized in process but also so involved. I answer the same questions the same way, every time. And we haven’t automated it. There are chronic diseases where we’re following patients over a long period of time. And there are somewhat standard interactions and communication cadences with these patients. If we can leverage machine learning to decrease the burden of documentation but also obtain that information, we can have more frequent, more valuable human connections.
Dr. Sugar: I agree that AI can be applied to colonoscopy preps. Computer aided detection of polyps during colonoscopy is rapidly expanding. It’s also used to identify if IBD patients are eligible for research studies. Patient engagement tools are still maturing, so making it easier for the patient to interact more seamlessly with the office is going to be key in the future.
Our Panel
Julie Servoss, MD, MPH, Senior Medical Director, Gastroenterology
Dr. Servoss is a board-certified gastroenterologist and internist who subspecializes in hepatology. She joined ModMed in 2014 and as Senior Medical Director of Gastroenterology, she helps code ModMed products while providing clinical input in terms of physician usability.
Jason Sugar, MD, CMO, Lead Gastroenterologist
Dr. Sugar started practicing gastroenterology in 2008, and is board-certified in Gastroenterology. He currently holds the Chief Medical Officer position at Washington Gastroenterology, as well as providing clinical input into ModMed products.
Sam Cicogna, General Manager, Gastroenterology
Sam joined ModMed in 2019 and brings 25 years of software implementation, project management, process design and technology leadership experience to his role in helping gastroenterology practices find technology solutions that fit their needs.
Chad Walker, National Sales Director, Gastroenterology
Chad joined ModMed in 2020 and has worked in healthcare for approximately 20 years, and in the gastroenterology space for five years.
This blog is intended for informational purposes only and does not constitute legal or medical advice. Please consult with your legal counsel and other qualified advisors to ensure compliance with applicable laws, regulations, and standards.
The statements and conclusions contained herein reflect the opinions of Julie Servoss, MD, MPH, Jason Sugar, MD, CMO, Sam Cicogna and Chad Walker, and not those of ModMed. ModMed makes no representations or warranties as to the accuracy of any such information.







