Specialty-Specific Value-Based Care
Driving Medicare Quality Payment Program Success With Solutions for MIPS
MIPS ADVISING RESULTS FOR EMA® USERS IN 2022*
%
of MIPS Advising clients met their score goals
99.3% Scored 75 points or more, avoiding penalties
*Numbers are estimated based on data collected by the Modernizing Medicine, Inc. Qualified Registry for the 2022 reporting year using the MIPS scoring criteria published by the Centers for Medicare & Medicaid Services (“CMS”); may not reflect scores for all MIPS categories; final results may vary. Prior performance doesn’t guarantee future results.
Why MIPS Performance Matters
Under the Merit-Based Incentive Payment System (MIPS), your Medicare reimbursement amount is driven, in part, by your ability to show high-quality and low-cost care as compared to your peers. If you need advisory services to help you achieve your goals, ModMed® has your back.
ModMed is a recognized leader in value-based care solutions for specialty practices, and now that 2022 MIPS is over, we’re proud to announce that our EMA providers achieved outstanding preliminary results.
How is your MIPS game?
A Built-in MIPS Solution
At ModMed, we have embraced the arrival of value-based care. As other practices and clinics struggle to meet the requirements, you can achieve your goals with our help.
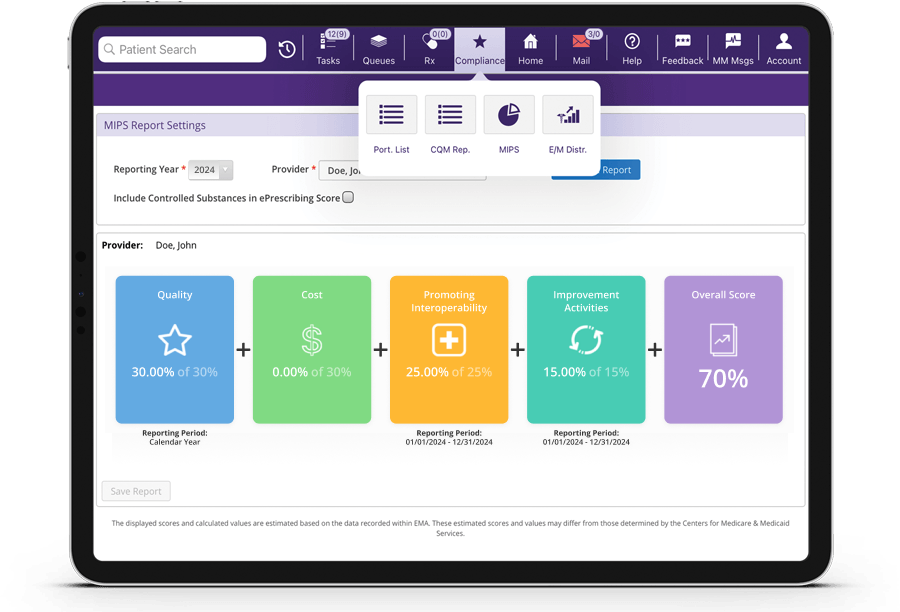
Our EHR, EMA, is certified according to the 2015 Edition Cures Update requirements, and our built-in MIPS solutions can help you gather and track your MIPS data:
- Collect MIPS data in the flow of the exam, without adding time or clicks.
- Track your estimated MIPS Composite Score and progress on each measure and category.
- Take advantage of our clinical data registries.
Why Choose ModMed?
Value-based care isn’t going away, and we know firsthand how time-consuming it can be to keep track of all the factors involved in MIPS reporting. That’s why we work hard to stay abreast of the changes. We can provide you with various solutions that fit your needs to help you achieve your MIPS goals:
- Industry leadership in specialty-specific EMR content and usability
- Built-in MIPS Composite Score tracking
- Patient collaboration tools, including patient kiosk, patient portal, patient reminders and patient surveys
- Concierge coaching with our advisory services*
- Web and mobile solutions
Make data-driven decisions to improve health and cost-effectiveness while succeeding under MACRA. Our powerful EMA EHR solutions dig deep into population trends, care utilization and various quality measure solutions, helping you stay competitive. By utilizing structured health-system-generated and patient-generated data, ModMed helps streamline workflows and gives you valuable insights that can drive achievement of your goals.
*Available at an additional cost.
MIPS and MACRA Explained
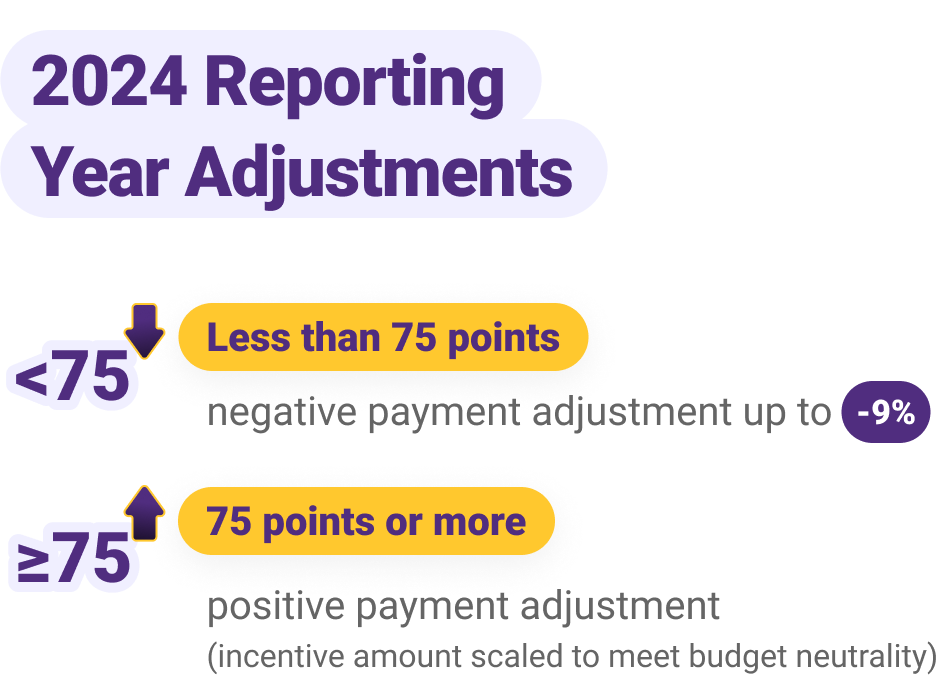
When the Medicare Access and CHIP Reauthorization Act (MACRA) became law in 2015, it immediately shifted the thought process behind Medicare payments. CMS wants to encourage physicians to provide high-quality, low-cost care. If you fail to report MIPS data to CMS, you could receive a negative payment adjustment.
THE EXCEPTIONAL PERFORMANCE BONUS IS NO LONGER AVAILABLE
However, there is still the possibility for a positive payment adjustment depending on your final score. For example, a score of 100% in 2022 yielded a positive payment adjustment of 8.25%.
MIPS puts your bottom line on the line
For the 2024 performance year, you can receive up to a 9% negative payment adjustment in 2026 (the payment year).
For example, if you bill $1.5 million per year in Medicare, your 2024 MIPS performance can make up to a $135,000 difference in your income in 2026.
Can you afford not to track your score?
As a leader in value-based medicine for specialty practices, ModMed can provide you with tools for MIPS success.
What makes up MIPS?
MACRA established the Quality Payment Program (QPP), which consolidated prior quality reporting programs and added a new component to create MIPS, with factors in four weighted performance categories:
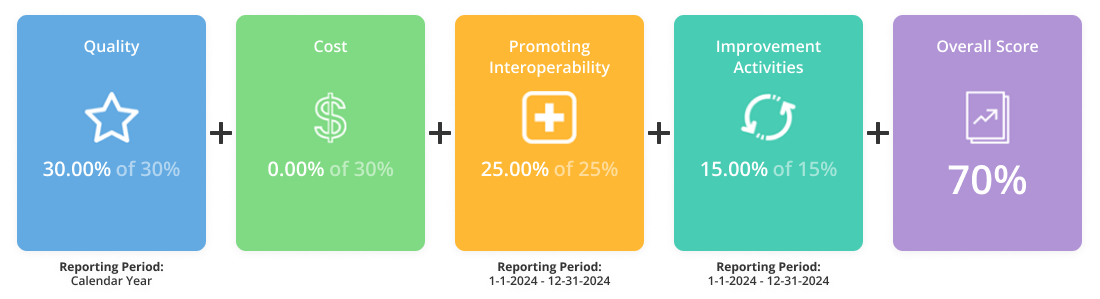
Data is key to helping you see where your practice stands in each performance category and where you may have room for improvement. Having an advanced EHR system like EMA to help automate your MIPS data collection and track your score will be crucial to the prosperity of your practice under value-based care.
We encourage you to visit CMS’ Quality Payment Program site to learn more about MIPS and MACRA.
The Future of MIPS (MVPs)
MIPS Value Pathways (MVPs) is a new optional way to report MIPS, which started in 2023. The goal of this program is to further reduce the administrative burden of MIPS on physicians and their staffs. It will only be available to certain specialties to start, but eventually it will replace traditional MIPS. If you plan to report to MVPs, you’ll need to register directly with CMS. We expect registration to open in April 2024.
Frequently Asked Questions
Can I see my overall MIPS score before submitting my data to CMS?
Yes, EMA calculates your estimated MIPS Composite Score nightly, providing you with visibility into your anticipated MIPS performance, both overall and in each individual category. For information on gGastro® EHR, please visit our gastroenterology value-based care page.
Where can I find more information on MIPS in EMA?
Visit ModMed Communities for other resources related to value-based care and EMA.
Does ModMed offer additional MIPS coaching resources?
Yes, we have an optional concierge-style coaching program called our MIPS Advisory Service that is available for an additional fee.
What is our EHR certification number?
For detailed information on our EHR certification, check out our ONC Health IT Disclosure page.
How can I submit MIPS data to CMS?
You can gather your Promoting Interoperability and Improvement Activities data from our EHR, EMA, and submit to the Quality Payment Program via attestation.


